Speakers' Corner - This month's personal view comes from Dr Sebastian Kalwij.

Dr Sebastian Kalwij has been involved with the Chlamydia screening programme in Lambeth, London, as GP Lead, since 2005 and as GP Lead for the National Chlamydia Screening Programme from 2009-2011. Additionally he has written the recent e-learning module on Sexual Health in Primary Care for the RCGP.
Being involved with Chlamydia screening at a National level I realised that though some Public Health targets are justifiable they are not always easy to implement. There are so many hurdles to overcome on a practical level. From using the right sample (urine vs self-taken swab) to using the right test request form, EMIS coding problems, laboratory feedback, patient management and partner treatment. On top of that the GP-landscape has changed dramatically.
Perhaps in the future this could be commissioned in a different way. Looking at the work done by GPs in Lambeth, primary care is certainly the right place to offer Chlamydia testing. GPs in Lambeth test more patients for Chlamydia than anywhere else in the country. Positivity rates remain high. The mantra; if you don’t look, you don’t find is certainly true. Over the years I followed my patients who were tested positive for Chlamydia trachomatis and though it is easy to treat, the after effects can be far reaching. Many a relationship has been destroyed because of it. One of my patients developed reactive arthritis in her knee and had to give up her career as a hairdresser.
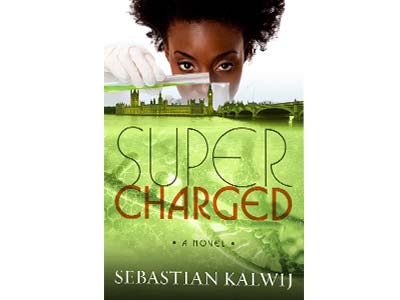
Motivating GPs and Nurses to test more patients on top of an already busy working day can be difficult, especially as it is not part of QOF, and I tried to come up with something novel. I find writing fiction a good way to de-stress in the evening and I decided to write a medical story ‘Supercharged’ around Chlamydia screening, soon it developed into a medical thriller. Perhaps a work of fiction can convince more people than merely presenting the facts.
Motivating GPs and Nurses to test more patients on top of an already busy working day can be difficult, especially as it is not part of QOF, and I tried to come up with something novel. I find writing fiction a good way to de-stress in the evening and I decided to write a medical story ‘Supercharged’ around Chlamydia screening, soon it developed into a medical thriller. Perhaps a work of fiction can convince more people than merely presenting the facts.
Sexual Health is broad term and defined by the WHO in 2006 as: “…a state of physical, emotional, mental and social well-being in relation to sexuality; it is not merely the absence of disease, dysfunction or infirmity. Sexual health requires a positive and respectful approach to sexuality and sexual relationships, as well as the possibility of having pleasurable and safe sexual experiences, free of coercion, discrimination and violence. For sexual health to be attained and maintained, the sexual rights of all persons must be respected, protected and fulfilled.”
From the definition it follows that most GPs will deal with most aspects of Sexual Health frequently.
In day to day practice Sexual Health means the following:
- Contraception. Negotiating the right contraception for each individual patient depends on many factors; age, BMI, smoking history, one’s stage in a relationship, interactions with medications and concurrent medical conditions. The right choice of contraception may change during a patient’s life too as personal circumstances change. Those at an increased risk of STI’s will need condoms in addition to their LARC or oral contraceptives (Double Dutch).
- Sexually Transmitted Infections. The list of STI’s is long, ranging from Scabies,Trichomonas, Gonorrhoea, Herpes and HPV to Hep B and C, Syphilis and HIV. In some cases patients may not always be aware of any symptoms whilst others, like herpes may present in a dramatic way. These consultations are never straightforward. You have to deal with the infection itself, sequelae, partner treatment and the impact it has on a patent’s relationship. When an infection has been aquired abroad you will have to discuss the right treatment with a microbiologist. Some infections are transient or easy to treat but others just change your patient’s life forever.
- Chlamydia screening. This should be offered to all patients < 25 who are having sex. The National Programme was rolled out in 2004 and since then millions of young people have been tested and treated. Chlamydia positivity remains high. In some areas as high as 8%. Chlamydia has been linked to PID, Tubal Factor Infertility, miscarriage and Reiter Syndrome. Tests are best offered opportunistically during a consultation. Treatment of Chlamydia is with a stat dose of Azithromycin.
- HIV testing in high risk areas. In areas of the UK where the HIV prevalence exceeds 2 in 1000 population (most inner city boroughs) routine HIV testing is recommended. 50% of HIV transmissions are from patients who are undiagnosed. As anti-retroviral medication is very effective, a near normal life-expectancy is achievable. But early diagnosis is the key and GPs must look out for so-called indicator signs.
- Sexual dysfunction, vaginismus, erectile dysfunction, sexual violence, FGM, sexual orientation and gender dysphoria. This is a broad field and GPs must make themselves familiar with secondary care referral pathways, support and save-havens. In some occasions liaison with adult and children social services or the police will be needed.
Issues related to sexual health carry a stigma and some patients have to pluck up courage to discuss this. When they do, it is important to be non-judgmental and have an open attitude.
Last updated : 17 Sep 2015Written response to GP partnership review (18 Sep 2018)
We have provided a written response to the GP Partnership Review which is being conducted for the Department of Health and Social Care by Dr Nigel Watson of Wessex LMCs....Tips of the month September 2018 (18 Sep 2018)
We provide weekly tips based on common queries which come through to us from London GPs and practice teams. These are shared via social media and collated for...Londonwide LMCs’ jobs board (18 Sep 2018)
Don’t forget our vacancies section is free to use for London practices. All you need to do is complete and submit the web form and we will do the rest...Winter pressures - keep us up to date (18 Sep 2018)
Last winter saw the whole health and social care system in London operating at full-stretch, with lack of capacity in secondary and social care increasing pressure on GPs. We are...LEAD Training Events (18 Sep 2018)
This year, our Learning Education and Development (LEAD) team created a new summer-time initiative for GPs and practice teams. Our LEAD Summer School programme ran throughout August and covered a...MMR and MenACWY vaccinations for students resident at home (17 Sep 2018)
September marks the time of the year when many students are starting their first year of university or returning to their studies. Students can be more vulnerable to illnesses such...How we use your data (17 Sep 2018)
In line with recent changes in data protection legislation, we have updated our Privacy Policy to provide you with more detail on how we handle your personal data. Our Privacy...Premises update September 2018 (14 Sep 2018)
This update is applicable to practices who are leasing their premises from Community Health Partnerships (CHP) or NHS Property Services (NHSPS). Urgent - Occupancy Agreement Letters We are aware that...Digital first consultation response (14 Sep 2018)
We have responded to NHS England’s consultation on ‘Digital-first primary care and its implications for general practice payments’. Our full response can be read here, a summary is...How to be a dementia friendly GP (14 Sep 2018)
There are currently 850,000 people in the UK with dementia, and this is set to rise to 1 million by 2025. We know that people with dementia can face challenges...Guidance
We provide expert guidance for practices in our guidance section, as well as an archive of other materials you may find useful.
GP Support
Contact our GP Support team if you need help or advice.
The team provide professional and pastoral support to GPs and practice teams on a broad range of issues.

