Speakers' Corner - This month's personal view comes from Dr Sebastian Kalwij.

Dr Sebastian Kalwij has been involved with the Chlamydia screening programme in Lambeth, London, as GP Lead, since 2005 and as GP Lead for the National Chlamydia Screening Programme from 2009-2011. Additionally he has written the recent e-learning module on Sexual Health in Primary Care for the RCGP.
Being involved with Chlamydia screening at a National level I realised that though some Public Health targets are justifiable they are not always easy to implement. There are so many hurdles to overcome on a practical level. From using the right sample (urine vs self-taken swab) to using the right test request form, EMIS coding problems, laboratory feedback, patient management and partner treatment. On top of that the GP-landscape has changed dramatically.
Perhaps in the future this could be commissioned in a different way. Looking at the work done by GPs in Lambeth, primary care is certainly the right place to offer Chlamydia testing. GPs in Lambeth test more patients for Chlamydia than anywhere else in the country. Positivity rates remain high. The mantra; if you don’t look, you don’t find is certainly true. Over the years I followed my patients who were tested positive for Chlamydia trachomatis and though it is easy to treat, the after effects can be far reaching. Many a relationship has been destroyed because of it. One of my patients developed reactive arthritis in her knee and had to give up her career as a hairdresser.
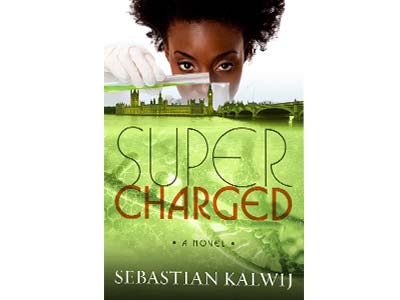
Motivating GPs and Nurses to test more patients on top of an already busy working day can be difficult, especially as it is not part of QOF, and I tried to come up with something novel. I find writing fiction a good way to de-stress in the evening and I decided to write a medical story ‘Supercharged’ around Chlamydia screening, soon it developed into a medical thriller. Perhaps a work of fiction can convince more people than merely presenting the facts.
Motivating GPs and Nurses to test more patients on top of an already busy working day can be difficult, especially as it is not part of QOF, and I tried to come up with something novel. I find writing fiction a good way to de-stress in the evening and I decided to write a medical story ‘Supercharged’ around Chlamydia screening, soon it developed into a medical thriller. Perhaps a work of fiction can convince more people than merely presenting the facts.
Sexual Health is broad term and defined by the WHO in 2006 as: “…a state of physical, emotional, mental and social well-being in relation to sexuality; it is not merely the absence of disease, dysfunction or infirmity. Sexual health requires a positive and respectful approach to sexuality and sexual relationships, as well as the possibility of having pleasurable and safe sexual experiences, free of coercion, discrimination and violence. For sexual health to be attained and maintained, the sexual rights of all persons must be respected, protected and fulfilled.”
From the definition it follows that most GPs will deal with most aspects of Sexual Health frequently.
In day to day practice Sexual Health means the following:
- Contraception. Negotiating the right contraception for each individual patient depends on many factors; age, BMI, smoking history, one’s stage in a relationship, interactions with medications and concurrent medical conditions. The right choice of contraception may change during a patient’s life too as personal circumstances change. Those at an increased risk of STI’s will need condoms in addition to their LARC or oral contraceptives (Double Dutch).
- Sexually Transmitted Infections. The list of STI’s is long, ranging from Scabies,Trichomonas, Gonorrhoea, Herpes and HPV to Hep B and C, Syphilis and HIV. In some cases patients may not always be aware of any symptoms whilst others, like herpes may present in a dramatic way. These consultations are never straightforward. You have to deal with the infection itself, sequelae, partner treatment and the impact it has on a patent’s relationship. When an infection has been aquired abroad you will have to discuss the right treatment with a microbiologist. Some infections are transient or easy to treat but others just change your patient’s life forever.
- Chlamydia screening. This should be offered to all patients < 25 who are having sex. The National Programme was rolled out in 2004 and since then millions of young people have been tested and treated. Chlamydia positivity remains high. In some areas as high as 8%. Chlamydia has been linked to PID, Tubal Factor Infertility, miscarriage and Reiter Syndrome. Tests are best offered opportunistically during a consultation. Treatment of Chlamydia is with a stat dose of Azithromycin.
- HIV testing in high risk areas. In areas of the UK where the HIV prevalence exceeds 2 in 1000 population (most inner city boroughs) routine HIV testing is recommended. 50% of HIV transmissions are from patients who are undiagnosed. As anti-retroviral medication is very effective, a near normal life-expectancy is achievable. But early diagnosis is the key and GPs must look out for so-called indicator signs.
- Sexual dysfunction, vaginismus, erectile dysfunction, sexual violence, FGM, sexual orientation and gender dysphoria. This is a broad field and GPs must make themselves familiar with secondary care referral pathways, support and save-havens. In some occasions liaison with adult and children social services or the police will be needed.
Issues related to sexual health carry a stigma and some patients have to pluck up courage to discuss this. When they do, it is important to be non-judgmental and have an open attitude.
Last updated : 17 Sep 2015What they said about the GP Essential Toolkit conference (05 Jul 2017)
Our first Essential Toolkit for GPs on Tuesday 4 July, 2017 was a huge success. See some of the top tweets from speakers and attendees below: ...GP volunteers needed for Grenfell Tower residents (22 Jun 2017)
Over the last few days we have seen a fantastic response to the Grenfell Tower fire from London GPs and practice teams, working in very difficult circumstances both practically and...Londonwide LMCs' June 2017 newsletter (21 Jun 2017)
...May 2017 workforce survey – thank you for responding (20 Jun 2017)
Our latest workforce survey closed on Tuesday 20 June, we received over 750 responses, representing over 550 practices. Thank you to those who took the time to provide us with...HR in general practice: recruitment and selection (16 Jun 2017)
Londonwide LMCs recently ran a recruitment and selection workshop for GPs and practice management colleagues. The day was full of lively discussion as delegates considered all aspects of the recruitment...Guest blog: Engaged patients boost your practice (16 Jun 2017)
This week (w/c 19 June) is patient participation awareness week. East London GP and LMC member Dr Naomi Beer tells us about the benefits of patient engagement and how it...General election 2017 – Summary of London results (15 Jun 2017)
Election night ended with a hung parliament and in London those boroughs represented by Londonwide LMCs saw Labour gain three seats from the Conservatives, Kensington, Battersea and Enfield Southgate. The...Fire at Grenfell Tower - assisting with relief work (15 Jun 2017)
Following on from the tragic events in Kensington yesterday morning, Londonwide LMCs is here to support you and your practice staff at this difficult time. Please remember look out for...CQC plans changes to inspection regime (15 Jun 2017)
The Care Quality Commission (CQC) has launched a consultation on proposals to change the general practice inspection regime to include practices providing annual written evidence on how they intend...Obituary: Dr Chris Jowett 19 August 1952 – 27 May 2017 (14 Jun 2017)
Last month we lost Dr Chris Jowett, the treasurer of our board, former vice-chair of Hillingdon LMC and a prolific advocate for London general practice for over three decades. This...Guidance
We provide expert guidance for practices in our guidance section, as well as an archive of other materials you may find useful.
GP Support
Contact our GP Support team if you need help or advice.
The team provide professional and pastoral support to GPs and practice teams on a broad range of issues.

